
If you’re in your 30s, 40s, or 50s, you may start having hot flashes or night sweats.
And hot flashes are frustrating, disruptive, and can feel so embarrassing– trust me I know!
As a woman reaching mid-life myself, I know how hot flashes can be a silent struggle. Many of us try to hide the fact that we have them, or even just laugh them away.
But keep in mind that they aren’t just a nuisance, they can actually be telling us more about our bodies.
More than 85% of women in the US will experience hot flashes and night sweats.
And our culture and previous generations of women tell us that hot flashes are a “normal” part of menopause. But what we need to realize is that they could be an indication that something else is wrong in the body.
A hot flash can mean your blood vessel lining may become damaged if your symptoms of perimenopause or menopause are untreated.
So how do we manage our perimenopause and menopause symptoms– like hot flashes– to keep our body balanced and in check?
Research shows a direct connection between blood sugar and hot flashes. So having low estrogen levels may no longer be the ONLY cause.
In this blog, we’ll discuss the relationship between blood sugar and hot flashes, and what you can do to help keep hot flashes at bay.
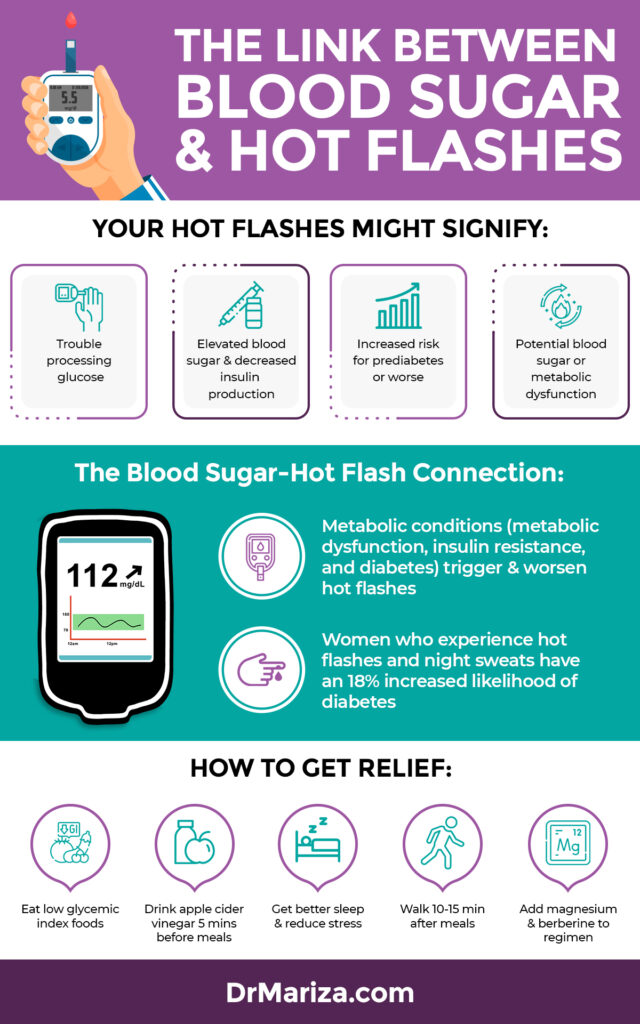
What Are Your Hot Flashes Really Telling You?
Hot flashes set off the autonomic nervous system, which is what regulates our basic bodily functions like temperature.
During a hot flash,
- Heart rate and blood flow to the skin increase
- Skin temperature spikes
- Then temperature plummets as the body starts giving off heat
The autonomic nervous system also plays a role in glucose regulation.
One theory is that the autonomic system changes during hot flashes are associated with increased glucose and decreased insulin production.
And remember, insulin is the essential hormone controlling our blood sugar levels.
Another hypothesis is that night sweats (aka hot flashes) disrupt sleep. So getting poor sleep can throw off our body’s ability to process glucose effectively.
An observation that may bolster this theory is that women whose symptoms lasted longer—meaning they had longer periods of disrupted sleep—had a greater risk of diabetes.
So you can see how blood sugar and hot flashes can go hand in hand.
Unstable blood sugar can lead to:
- Metabolic issues
- Weight gain
- Poor sleep
- and the hormonal symptoms we experience in menopause
So if one of the potential root causes of hot flashes is unstable blood sugar, we have a pretty good idea of how to tackle it.
What’s the Research Between Blood Sugar and Hot Flashes?
Metabolic conditions like metabolic dysfunction, insulin resistance, and diabetes (which are at an ALL-TIME high) seem to make hot flashes worse, suggesting blood sugar and hot flashes are related.
Glucose levels in our body can be impacted by everything from:
- Daily sleep
- Exercise
- Diet
- Stress levels
Glucose is also influenced by overall insulin sensitivity– which is how responsive your cells are to insulin. Insulin resistance is when your cells don’t respond to insulin appropriately, so there’s an issue in taking up glucose from the bloodstream.
As many as 88% of women already have some form of metabolic dysfunction, whether it’s unstable blood sugar, high triglycerides, or high blood pressure.
So metabolic dysfunction can be a root cause of experiencing increased hot flashes.
Here’s how blood sugar links up to hot flashes in research:
- A study of about 150,000 postmenopausal women, followed over 20 years, linked hot flashes and night sweats with an 18% increased likelihood of diabetes. The correlation was higher in patients with more frequent and severe symptoms.
- Another study of more than 3,000 overweight women followed for eight years linked hot flash symptoms to higher insulin resistance and fasting blood glucose levels.
- In a study of 17,000 postmenopausal women, researchers saw that eating a blood sugar-balanced diet low in fat and high in vegetables, fruits, and whole grains can decrease hot flash frequency.
- Some studies have seen people experience fewer hot flashes after eating, and more hot flashes when blood glucose falls between meals. That’s likely because changing estrogen levels cause a drop in the amount of a glucose-transporting protein made in the blood-brain barrier.
What we see as doctors is that this blood sugar roller coaster ends up leading to metabolic dysfunction, diabetes, and ultimately, more severe menopause symptoms– including hot flashes.
Why BOTH High and Low Blood Sugar Are a Problem
Women who experience hot flashes tend to be more likely to develop insulin resistance, yet those same people tend to have higher glucose levels.
These changes decrease the rate at which glucose is transported into the brain, causing dips in its energy resources.
And this lack of energy activates the autonomic nervous system which triggers a hot flash– releasing glucose and providing the brain much needed fuel.
Progesterone declines and estrogen soars in perimenopause, then estrogen falls in menopause– causing your brain not to use glucose as efficiently as it once did.
So when your blood sugar is low, you’re REALLY low.
But at the same time, insulin resistance in the brain makes it harder for brain cells to transport glucose into brain cells to produce energy.
So even though someone with insulin resistance may have more glucose in their blood, that extra glucose still may not be making it to the brain to supply adequate energy.
How to Improve Insulin Sensitivity & Metabolic Function
Pumping yourself full of glucose just to get it into the brain is not the best solution. Instead, your goal should be to improve insulin sensitivity and get off the blood sugar roller coaster– now and for good.
Spikes and dips in blood glucose tend to promote insulin resistance over time and stimulate the autonomic stress response in the body. And we know how this response is linked to hot flashes!
So, if the goal is to improve insulin sensitivity, then how do you do it?
Weight loss and healthy diets improve insulin sensitivity, which promotes better glucose control.
Here are a few of my favorite tips to improve insulin sensitivity and metabolism:
- Choose foods with a low glycemic index, like fruits, vegetables, and whole grains
- Drink Apple Cider Vinegar before meals
- Improve your sleep
- Manage your stress
- Exercise regularly
- Consider Supplements and herbs
Sometimes even lifestyle changes are not enough. So certain supplements can help accelerate your results.
My Essentially Whole Magnesium Restore supplement helps your body find more balance, leaving you energized and less stressed all day.
And my Essentially Whole Gluco Support supplement supports a healthy balance in blood sugar, getting you off the blood sugar rollercoaster and boosting your all-day energy!
All of these tips over time can allow the brain to be more responsive to the glucose circulating in your body– ultimately minimizing hot flashes.
How to Control Your Blood Sugar So You Can Reduce Hot Flashes
Maintaining stable glucose levels consistently over time through a healthy diet, natural supplements like my Gluco Support, and lifestyle modifications may be your best bet for managing menopause symptoms like hot flashes.
So check out my podcast: 5 Easy Ways to Fix Your Blood Sugar, and my free guide– 5 Hacks to Blunt a Blood Sugar Spike.
Both of these resources are jam-packed with my top recommendations for keeping your blood sugar balanced, helping to decrease those frustrating menopausal hot flashes.
And as you start to make the simple lifestyle changes needed, I highly recommend you also add the two key supplements I mentioned above to your regimen– Magnesium Restore and Gluco Support.
Both supplements will vastly improve your body’s ability to balance your blood sugar. And in turn, keep away metabolic dysfunction and the worst symptoms of menopause, including hot flashes.
Getting your blood sugar under control will dramatically improve your quality of life, decrease the severity of your symptoms, and even ease your transitions through perimenopause and menopause.
Plus, you’ll stay metabolically healthy and insulin sensitive. This helps you avoid metabolic dysfunction and other related health issues.
To get the most out of your life and to take your metabolism journey even further, join me for a full-on metabolic makeover in my Metabolism and Hormone Reset Course!
I’m here for you through every phase of your life, and I’m excited to continue to help you feel like your healthiest self.
Get My 5 Hacks to Block Blood Sugar Spikes!
You’re exhausted. Your brain’s fried. Your weight’s creeping up… It’s not you — it’s your blood sugar! Finally, a simple answer and an easy fix in just 5 STEPS. Download Dr. Mariza’s Self-Care Guide Here

No comments yet.